Autoimmune disorders occur when a dog’s own protective cells mistakenly attack its body. When this condition targets the skin’s epidermis and dermis, these layers can separate, leading to painful, blistering lesions. This article delves into the causes, diagnosis, and treatment of these complex conditions, drawing from expert insights and research.
Understanding Autoimmune Skin Eruptions
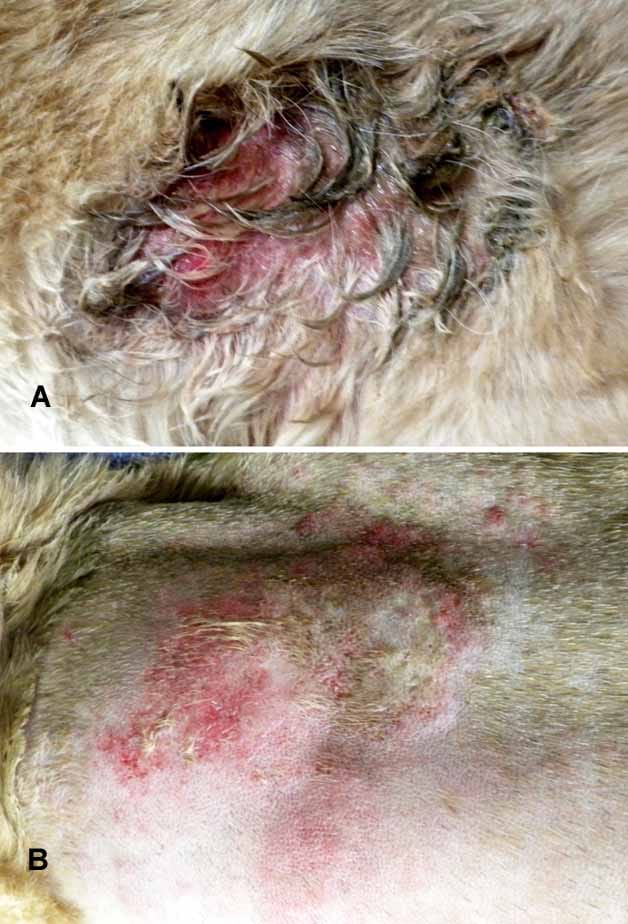
In autoimmune skin diseases, the separation of skin layers can result in the formation of blisters and pustules. These fragile areas are prone to erosion, crusting from discharged fluid, and subsequent hair loss. Secondary bacterial infections are a common complication, further compromising the skin’s integrity. Severe and recurring cases of atopic dermatitis are frequently implicated, making dogs susceptible to autoimmune skin problems. Symptoms of atopic dermatitis often include persistent itching, sneezing, rashes, watery eyes, and excessive paw chewing. By the time a definitive diagnosis is made, the initial trigger may have long passed, complicating the diagnostic and treatment process.
While viruses are known triggers for autoimmune skin conditions in humans, their role in dogs is less documented. Genetic predisposition, a known factor in human autoimmune disorders, is suspected but not definitively proven in dogs. For instance, superficial pemphigus is observed more frequently in certain breeds, such as the Akita.
Certain medications can also act as triggers in individual dogs. These include antibiotics like sulfonamide, penicillin, and cephalosporin, as well as topical medications for external parasite control, such as those containing fipronil, amitraz, S-methoprene, dinotefuran, pyriproxyfen, or permethrin. In such cases, discontinuing the medication may resolve the skin issues. However, other dogs require ongoing treatment to restore and maintain healthy skin.
Diagnosing Autoimmune Skin Diseases in Dogs
Although not common, autoimmune skin diseases do occur in dogs. A comprehensive medical history is crucial to rule out drug-induced conditions and parasitic infections as potential causes of the skin lesions. When other causes are eliminated, a skin biopsy becomes the definitive diagnostic tool.
However, obtaining a suitable biopsy can be challenging. Ideally, a vesicle or pustule should be captured before it erodes, but these lesions are delicate and rarely intact when a biopsy is attempted. Furthermore, any prior treatment can skew biopsy results. As one expert notes, even with extensive experience, an autoimmune skin disease cannot be definitively diagnosed without a biopsy.
The expense of biopsies can be a significant factor, sometimes leading veterinarians to initially try steroid treatments. If steroids prove insufficient or lesions reappear after discontinuation, a biopsy may then be pursued. A major drawback of this approach is the required 14 to 21-day waiting period without steroids before a biopsy can be taken, to avoid altering the histological findings and potentially leading to an incorrect diagnosis.
Effective Treatment Strategies
Generally, a combination of medications yields faster results and reduces the risk of side effects compared to high doses of individual drugs. Treatment protocols often begin with glucocorticoids (steroids like prednisone), either alone or in conjunction with potent immunosuppressive medications such as azathioprine or cyclosporine.
While steroids are cost-effective and easy to administer, long-term use can lead to side effects, including increased thirst and urination, and potentially more serious conditions like diabetes mellitus, liver disease, and Cushing’s disease. Pulse therapy, involving intermittent administration of large steroid doses, may be employed, particularly in initial high-dose treatments, followed by periodic dosing instead of daily lower doses. For milder or localized issues, topical steroids or immunomodulators like tacrolimus may be sufficient for temporary remission.
Antibiotics are often necessary to combat secondary bacterial infections that thrive in compromised skin. A culture and sensitivity test is recommended to identify the most effective antibiotic. Dogs suffering from atopy or other allergic dermatitis conditions benefit from concurrent treatment of these underlying issues, as well as any secondary yeast or fungal infections.
Emerging treatments for canine autoimmune skin disease include acupuncture, sometimes combined with herbal therapies. Oclacitinib (Apoquel) shows promise, though further research is needed before widespread recommendation. A key advantage of oclacitinib is its generally milder side effect profile and improved safety compared to long-term corticosteroid use.
Some dogs may achieve remission for varying periods, allowing for weaning to lower medication doses or even complete cessation of medication. However, the disease often recurs. It’s also important to note that while shampooing might seem beneficial, it can sometimes exacerbate the condition. Commercial shampoos may contain low concentrations of hydrocortisone, and the mechanical action of bathing and rinsing can irritate fragile autoimmune skin, potentially worsening the condition.
Types of Canine Autoimmune Skin Diseases
This article has been reprinted with permission from the Cornell University College of Veterinary Medicine’s DogWatch newsletter. When you become a member of the Riney Canine Health Center, you will receive a free subscription to DogWatch.