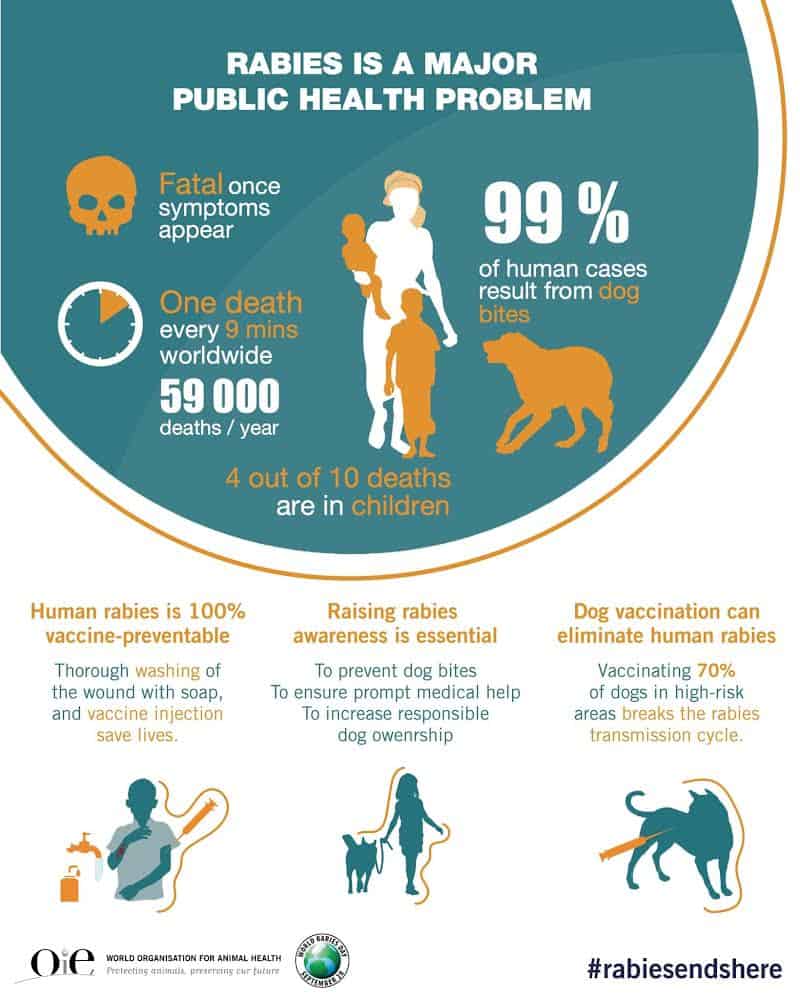
Rabies remains a significant global public health concern, affecting over 150 countries and territories, with a disproportionate impact on Asia and Africa. This viral, zoonotic, and often neglected tropical disease claims tens of thousands of lives annually, with a tragic 40% of victims being children under the age of 15. The primary mode of transmission to humans, accounting for 99% of cases, is through bites and scratches from infected dogs. Fortunately, dog vaccination and effective bite prevention strategies offer a powerful defense against this deadly disease. While rabies is invariably fatal once clinical symptoms manifest, prompt post-exposure prophylaxis (PEP) can effectively halt the virus’s progression to the central nervous system. PEP encompasses thorough wound washing, a course of human rabies vaccine, and, when necessary, rabies immunoglobulins. Therefore, immediate medical attention following any bite or scratch from a potentially rabid animal is paramount. Recognizing this, the World Health Organization (WHO) and its global partners are committed to eliminating human deaths from dog-mediated rabies through a comprehensive One Health approach, emphasizing mass dog vaccination, ensuring access to PEP, training healthcare professionals, enhancing surveillance, and promoting community awareness for bite prevention.
Understanding Dog-Mediated Rabies
Rabies is a vaccine-preventable viral disease that affects the central nervous system of mammals, including dogs, cats, livestock, and wildlife. Transmission to humans predominantly occurs through the saliva of infected animals, typically via bites, scratches, or direct contact with mucous membranes, such as the eyes, mouth, or open wounds. Once the virus invades the central nervous system and clinical signs emerge, rabies is virtually 100% fatal. The economic burden of rabies is substantial, estimated at US$8.6 billion annually, encompassing lost lives, diminished livelihoods, medical expenses, and unquantified psychological distress. While rabies is present on all continents except Antarctica, with an estimated 59,000 annual deaths globally, underreporting means documented cases often fall short of this figure. As a neglected tropical disease (NTD), rabies disproportionately affects marginalized populations who often face barriers to accessing effective human vaccines and immunoglobulins. The average estimated cost of rabies post-exposure prophylaxis (PEP), including travel and lost income, can be around US$108, posing a significant financial challenge for individuals living on US$1–2 per day. Despite these challenges, over 29 million people worldwide receive the human rabies vaccine each year.
Rabies Transmission Beyond Dogs
In the Americas, where dog-mediated rabies has been largely controlled, hematophagous bats have emerged as the primary source of human rabies infections. Bat-mediated rabies also presents a growing public health threat in Australia and parts of western Europe. While human deaths from encounters with foxes, raccoons, skunks, and other wild mammals are exceedingly rare, and bites from rodents are not known to transmit rabies, caution is always advised. Extremely rare instances of rabies transmission have occurred through inhalation of virus-containing aerosols, consumption of raw meat or milk from infected animals, or organ transplantation. Human-to-human transmission through bites or saliva is theoretically possible but has never been definitively confirmed.
Recognizing Rabies Symptoms
The incubation period for rabies typically ranges from two to three months but can vary significantly, from one week to over a year, influenced by factors such as the site of viral entry and the viral load. Initial symptoms are often non-specific, including fever, pain, and unusual sensations like tingling, pricking, or burning at the wound site. As the virus progresses to the central nervous system, it causes severe and ultimately fatal inflammation of the brain and spinal cord. While clinical rabies can be managed, complete recovery without severe neurological deficits is exceptionally rare.
Rabies presents in two main forms:
- Furious Rabies: Characterized by hyperactivity, extreme excitability, hallucinations, loss of coordination, hydrophobia (fear of water), and aerophobia (fear of drafts or fresh air). Death typically occurs within days due to cardiorespiratory arrest.
- Paralytic Rabies: Accounts for approximately 20% of human cases and follows a less dramatic, typically longer course. Muscles progressively weaken, beginning at the wound site, leading to a slow-onset coma and eventual death. This form is often misdiagnosed, contributing to under-reporting.
Diagnosing Rabies
Currently, there are no WHO-approved diagnostic tools for detecting rabies infection before the onset of clinical symptoms. Clinical diagnosis can be challenging without a confirmed history of contact with a rabid animal or specific symptoms like hydrophobia or aerophobia. Therefore, accurate risk assessment is crucial in determining the necessity of PEP. Once symptoms appear and are inevitably fatal, providing comprehensive and compassionate palliative care is recommended. Postmortem confirmation of rabies infection is achieved through various laboratory techniques that detect viral presence in infected tissues. Where feasible, testing the biting animal is also advised.
Preventing Rabies: A Multi-faceted Approach
Dog Vaccination: The Cornerstone of Prevention
The most effective and cost-efficient strategy for preventing human rabies is mass dog vaccination programs. By vaccinating dogs, including puppies, the transmission cycle is broken at its source. It is important to note that culling free-roaming dogs has proven ineffective in rabies control.
Public Awareness and Education
Public education campaigns targeting both children and adults are essential components of rabies prevention. These initiatives should cover dog behavior and bite prevention techniques, guidance on actions to take if bitten or scratched by a potentially rabid animal, and promoting responsible pet ownership.
Human Vaccination Strategies
Effective vaccines are available for both pre-exposure and post-exposure immunization in humans. As of 2024, three WHO pre-qualified human rabies vaccines are available globally: RABIVAX-S by Serum Institute of India Pvt. Ltd., VaxiRab N by Zydus Lifesciences Limited, and VERORAB by Sanofi Pasteur.
Pre-exposure Prophylaxis (PrEP): Recommended for individuals in high-risk occupations, such as laboratory workers handling live rabies viruses, and those whose professional or personal activities involve potential contact with infected animals, like animal disease control staff and wildlife rangers. PrEP may also be considered for recreational activities or travel in certain high-risk areas, or for individuals residing in remote, rabies-endemic regions with limited access to medical care. It is crucial to remember that PrEP does not negate the need for PEP following an exposure.
Post-exposure Prophylaxis (PEP): This is the critical emergency response to a potential rabies exposure, designed to prevent the virus from reaching the central nervous system. A thorough wound risk assessment and appropriate PEP protocol involve:
- Immediate and thorough washing of the wound with soap and water for at least 15 minutes.
- A course of rabies vaccine.
- Administration of rabies immunoglobulin or monoclonal antibodies into the wound, if indicated.
The necessity and type of PEP are determined by the category of exposure:
| Categories of contact with suspect rabid animal | Post-exposure prophylaxis measures |
|---|---|
| Category I: Touching or feeding animals, licks on intact skin. | Washing of exposed skin surfaces; no PEP required. |
| Category II: Minor scratches or abrasions without bleeding, nibbling of uncovered skin. | Wound washing and immediate vaccination. |
| Category III: Single or multiple transdermal bites or scratches, contamination of mucous membrane or broken skin with saliva, exposures involving bats. | Wound washing, immediate vaccination, and administration of rabies immunoglobulin/monoclonal antibodies. |
Category II and III exposures necessitate human rabies vaccination.
Ensuring Vaccine Quality and Administration
The WHO strongly recommends that all human rabies vaccines adhere to WHO standards. The deployment of substandard rabies vaccines has unfortunately led to public health failures in several countries.
Regarding vaccine administration, the WHO advocates for a transition from intramuscular (IM) to intradermal (ID) administration of human rabies vaccines. This method reduces the required vaccine volume and the number of doses, consequently lowering costs by 60–80% without compromising safety or efficacy. Furthermore, fewer doses enhance patient compliance with the recommended treatment regimen.
WHO’s Commitment to Rabies Elimination
Rabies is a key focus within the WHO’s 2021–2030 Roadmap for the global control of Neglected Tropical Diseases (NTDs). This roadmap sets ambitious regional and global targets aimed at eradicating human deaths from dog-mediated rabies by 2030. Key initiatives include:
- Enhancing access to human rabies vaccines: Through collaborative efforts with partners like Gavi, the Vaccine Alliance, the WHO is working to improve vaccine accessibility.
- Providing technical guidance: Supporting countries in developing and implementing national rabies elimination plans, with a focus on strengthening surveillance and reporting systems.
- Building workforce capacity: Encouraging countries to develop their One Health workforce by leveraging rabies elimination programs as platforms for multisectoral collaboration.
- Promoting the United Against Rabies (UAR) forum: This multi-stakeholder platform, established in collaboration with the Food and Agriculture Organization (FAO) and the World Organisation for Animal Health (WOAH), serves to advocate for increased action and investment in rabies control.