When your canine companion develops unusual skin eruptions, it can be a cause for concern. These spontaneous, nasty lesions might be indicative of an underlying autoimmune disorder, a complex condition where the dog’s own immune system mistakenly attacks healthy tissues. This article delves into the nature of autoimmune skin diseases in dogs, their diagnosis, and potential treatment avenues, drawing insights from veterinary experts.
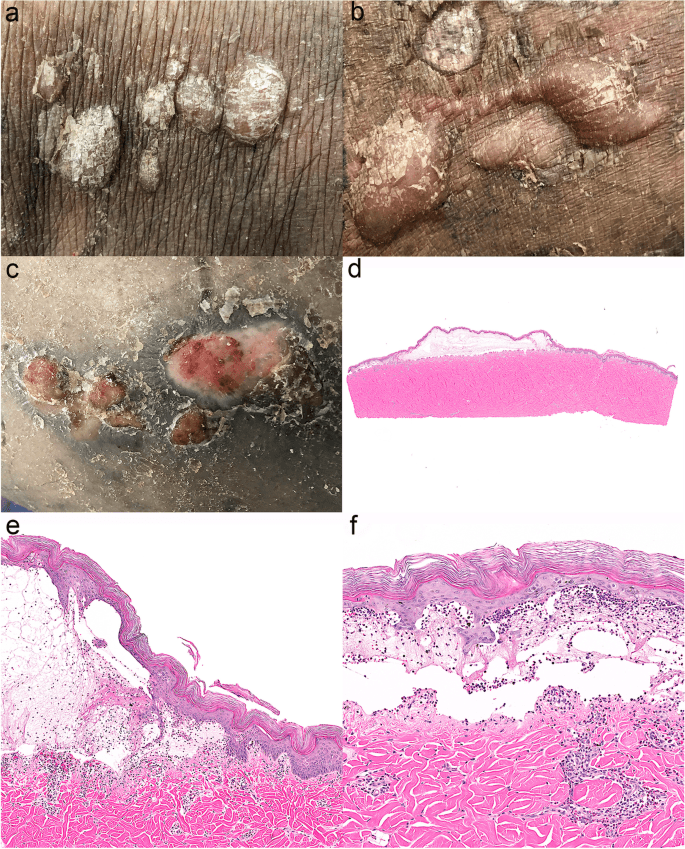
Autoimmune disorders occur when the body’s defense mechanisms, designed to fight off external threats, turn inward and attack the dog’s own cells. When this aberrant immune response targets the skin’s epidermis and dermis, it can lead to a separation of these layers, resulting in painful, blistering lesions. As the skin layers part, fluid-filled blisters and pustules may form. These fragile areas are prone to erosion, crusting from discharge, and subsequent hair loss. Secondary bacterial infections are also a common complication, further exacerbating the skin’s condition.
While the exact triggers for autoimmune skin diseases in dogs are not always clear, certain factors are suspected. Severe, recurring cases of atopic dermatitis (allergies) can predispose a dog to developing autoimmune skin problems. Symptoms of atopy often include persistent itching, sneezing, skin rashes, watery eyes, and excessive paw licking. Unfortunately, by the time a definitive diagnosis is made, the initial trigger may have long since passed, complicating the diagnostic and treatment process. In humans, viruses are known to trigger autoimmune skin conditions, but their role in dogs is less documented. While a genetic predisposition is recognized in human autoimmune disorders, its direct influence in canine counterparts is still under investigation. However, some breeds may be more susceptible; for instance, superficial pemphigus is observed more frequently in breeds like the Akita.
In some individual dogs, certain medications can act as triggers. This includes antibiotics such as sulfonamide, penicillin, and cephalosporin. Topical treatments designed to control external parasites, containing ingredients like fipronil, amitraz, S-methoprene, dinotefuran, pyriproxyfen, or permethrin, have also been implicated. In cases where a medication is the culprit, discontinuing the drug may allow the skin to return to normal. For other dogs, however, ongoing treatment is necessary to manage and maintain healthy skin.
Diagnosis of Autoimmune Skin Diseases
Although not exceedingly common, autoimmune skin diseases do occur in dogs. A comprehensive medical history is crucial to rule out drug-induced conditions and parasitic infestations as the cause of the lesions. If these possibilities are excluded and the cause remains elusive, a skin biopsy may be necessary for a definitive diagnosis.
Performing a skin biopsy can be challenging. Ideally, the biopsy should be taken from an intact vesicle or pustule before it erodes. However, these lesions are extremely delicate and rarely found in a suitable state for biopsy in time. Furthermore, any prior treatment can interfere with and alter the biopsy results. As Dr. William H. Miller Jr., professor emeritus of medicine, notes, “Even with my 40 years of experience, I can’t absolutely tell you that your dog has an autoimmune skin disease without the biopsy”.
The biopsy procedure can be costly. In situations where financial constraints are a factor, a veterinarian might initially opt for a trial of steroids. If the steroids provide insufficient relief or if the lesions reappear once the medication is stopped, a biopsy may then be considered. A significant caveat to this approach is that steroids cannot be administered for 14 to 21 days prior to the biopsy, as their presence can skew the histological results and potentially lead to an incorrect diagnosis.
Treatment Strategies for Canine Autoimmune Skin Diseases
Typically, a combination of medications yields the most rapid results. Using lower doses of individual drugs can also help minimize the risk of adverse side effects. Most treatment protocols commence with glucocorticoids (steroids like prednisone), either alone or in conjunction with potent immunosuppressive agents such as azathioprine or cyclosporine (Atopica).
Steroids are relatively inexpensive and easy for owners to administer at home. However, long-term use can lead to side effects. These can range from increased thirst and urination to more serious conditions like diabetes mellitus, liver disease, and Cushing’s disease (iatrogenic hyperadrenocorticism). Pulse therapy, involving intermittent administration of high doses, may be employed, particularly when dogs initially receive high steroid dosages, followed by periodic rather than daily dosing. For milder or localized issues, topical steroids or immunomodulators (medications that help regulate the immune system) like tacrolimus might be effective in managing the disease in remission, at least temporarily.
Antibiotics may be necessary to combat secondary bacterial infections that can flourish in compromised skin. A culture and sensitivity test is recommended to identify the most effective antibiotic. Dogs suffering from atopy or other allergic dermatitis conditions will benefit from concurrent treatment of these underlying issues. The same applies to secondary yeast or fungal infections.
Emerging treatment options for canine autoimmune skin disease include acupuncture, potentially combined with herbal therapies such as radix Curcuma wenyujin, Tripterygium wilfordii, Artemisia annua, and Berberis vulgaris. Oclacitinib (Apoquel) shows promise, though further research is needed before its widespread recommendation. A significant advantage of oclacitinib is its generally milder side effect profile and higher overall safety compared to long-term corticosteroids.
Some dogs may achieve remission for varying periods, allowing for a reduction in medication dosage or even a complete cessation of treatment for a time. However, in most cases, the disease is likely to recur.
Finally, while it might be tempting to bathe your dog, it is often best to refrain from shampooing during active flare-ups. “Shampoos have several problems,” explains Dr. Miller. “First, the commercially available ones contain 1% hydrocortisone, which isn’t very potent. The second issue with shampoos is that they can make things worse by the mechanical action needed to apply them and rinse them off. Autoimmune skin is more fragile than normal, and rubbing and rinsing can make it worse”.
If your dog is experiencing unusual skin lesions, consult your veterinarian for a proper diagnosis and a tailored treatment plan. Early intervention and appropriate management are key to ensuring your dog’s comfort and well-being. For more in-depth information on canine health, consider becoming a member of the Riney Canine Health Center, which includes a subscription to their DogWatch newsletter.