Pyometra is a serious and potentially life-threatening uterine infection affecting intact (unspayed) female dogs, often striking middle-aged to elderly pets. As loving dog owners, understanding this condition, its treatment, and the role of Pyometra Antibiotics is crucial for ensuring the best possible care for our canine companions. While surgery remains the most effective treatment, the use of antibiotics, both before and after the procedure, is a complex topic often lacking clear guidelines. This can lead to varied practices among veterinarians and contributes to the growing concern of antimicrobial resistance.
A recent survey conducted among veterinarians in Arizona shed light on current practices regarding antibiotic use in surgically treated canine pyometra cases. This study aimed to identify common patterns of antimicrobial prescription and culture submission, highlighting areas where clearer guidelines are desperately needed to optimize patient care and combat the global threat of antibiotic resistance. For dog owners, these insights are vital for informed discussions with your vet about your pet’s treatment plan.
What is Pyometra and Why is it a Concern for Dog Owners?
Pyometra is essentially a severe uterine infection characterized by the accumulation of pus within the uterus. This condition is remarkably common, affecting 20% to 25% of intact female dogs by the age of 10 years. It typically develops during the dioestrus phase of the estrous cycle (the period following heat), when the uterus is under the influence of progesterone. Progesterone makes the uterine lining thicker and more secretory, while also reducing uterine contractions. These changes create a perfect environment for bacteria, most commonly Escherichia coli (E. coli), to ascend from the vagina and cause a serious infection.
The consequences of pyometra can be severe. If left untreated, the uterus can rupture, leading to peritonitis (inflammation of the abdominal lining), sepsis (a life-threatening systemic infection), and even death. Early diagnosis and prompt treatment are paramount for a positive outcome….
The Role of Antibiotics in Pyometra Treatment
The most definitive and effective treatment for pyometra is an ovariohysterectomy (surgical removal of the uterus and ovaries), which eliminates the source of infection and inflammation. While this procedure is generally considered a “clean” surgery for uncomplicated cases, pyometra presents a unique challenge due to the presence of an active, often severe, infection within the body.
The use of pyometra antibiotics is a critical component of managing the infection, but when and how they should be used is often debated among veterinary professionals. Antibiotics can be administered:
- Preoperatively: Before surgery to stabilize a systemically ill patient and reduce the bacterial load.
- Perioperatively: During surgery to prevent infection in the surgical site.
- Postoperatively: After surgery to address any remaining systemic infection or potential contamination…
Historically, anecdotal evidence has suggested the use of antibiotics for dogs that are significantly ill, have a concurrent urinary tract infection, or experience complications during surgery. However, robust prospective studies supporting specific recommendations for pyometra cases have been lacking. Medical management using hormone therapy can sometimes be an option, but success rates are moderate, and antibiotics alone are often insufficient without surgical intervention, possibly due to bacterial biofilms in the uterus that resist treatment.
The broader concern of antimicrobial resistance looms large in veterinary medicine, mirroring a similar crisis in human medicine. Overuse or inappropriate use of antibiotics accelerates the development of resistant bacterial strains, making future infections harder to treat. This is why veterinary organizations advocate for judicious use of antimicrobials and emphasize techniques like de-escalation (starting with broad-spectrum antibiotics and then narrowing to more specific ones once culture results are available). In the context of pyometra, an ovariohysterectomy removes the infected organ, potentially negating the need for extensive or prolonged antibiotic therapy in some cases. However, clear, evidence-based guidelines for pyometra antibiotics have been notably absent compared to other common canine infections like urinary tract or respiratory infections.
This lack of precise guidance risks both the development of resistance and increased treatment costs for pet owners. The Arizona survey aimed to bridge this knowledge gap by documenting current practices, hoping to encourage the development of clearer, evidence-based protocols.
Key Findings from a Recent Veterinary Survey on Antibiotic Use for Pyometra
To understand current veterinary practices, a detailed survey was distributed to 863 small and mixed animal veterinarians in Arizona, resulting in 152 responses. The survey investigated demographics, patterns of antibiotic use, rates of bacterial culture submission, and outcomes of surgically treated pyometra cases.
Demographics of Participating Veterinarians
The majority of respondents were seasoned practitioners: 64% had over 10 years of experience, while 88% worked in general practice. Most veterinarians (66%) exclusively treated cats and dogs, and 58% practiced in suburban areas.
High Prevalence of Antibiotic Use
A significant finding was the widespread use of pyometra antibiotics among the surveyed veterinarians:
- 76% stated they always used preoperative and perioperative antibiotics.
- 74% stated they always used postoperative antibiotics.
This indicates that a large percentage of dogs undergoing pyometra surgery receive antimicrobial therapy, often routinely. This contrasts with some previous studies reporting lower rates of antibiotic use in pyometra cases.
Diversity in Antibiotic Choice and Duration
The survey identified the use of 16 different types of antibiotics. The four most commonly reported were:
- Amoxicillin/clavulanate potassium (86%): A broad-spectrum antibiotic often used for various bacterial infections.
- Enrofloxacin (52%): A fluoroquinolone antibiotic, effective against a range of bacteria.
- Cefazolin (37%): A first-generation cephalosporin, commonly used perioperatively.
- Ampicillin/sulbactam (22%): A combination antibiotic effective against certain resistant bacteria.
Interestingly, patterns of antibiotic choice varied based on demographic factors:
- Veterinarians with more than 10 years of experience were less likely to use ampicillin/sulbactam.
- Specialty practitioners and those working exclusively with cats and dogs were more likely to use ampicillin/sulbactam.
- General practitioners and those without additional training were more likely to use cefazolin.
Regarding the duration of postoperative pyometra antibiotics, there was considerable variability, ranging from 2 to 30 days. Many practitioners admitted that their chosen duration was arbitrary, despite some reporting adherence to “manufacturing guidelines” or “documented doses.” This lack of standardized duration highlights a significant gap in specific treatment protocols.
The Critical Importance of Bacterial Culture & Sensitivity Testing
Perhaps one of the most concerning findings was the low rate of bacterial culture submission. Only 12% of respondents regularly (always or usually) submitted a culture from the infected uterus.
Reasons for Not Submitting a Culture
Veterinarians cited several key reasons for not performing cultures:
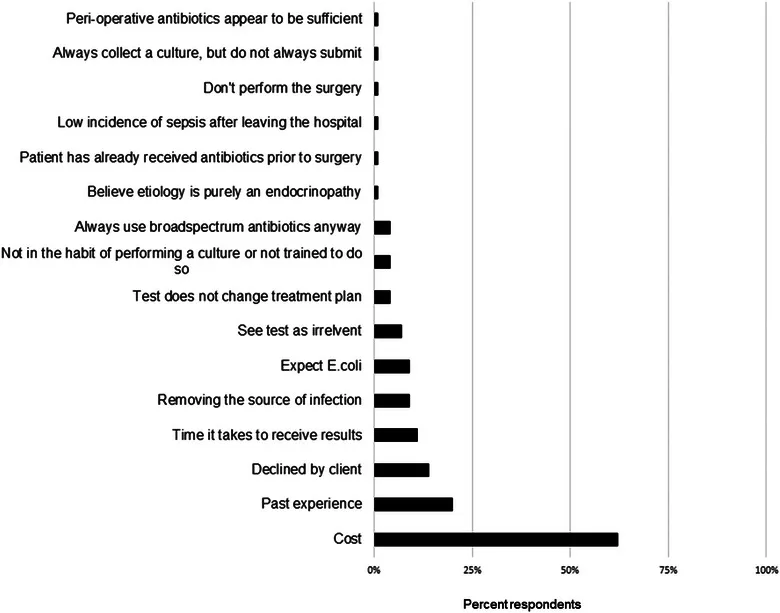 Common reasons veterinarians cite for not performing bacterial culture for canine pyometra, including cost and turnaround time
Common reasons veterinarians cite for not performing bacterial culture for canine pyometra, including cost and turnaround time
- Cost of the test (63%): This was the most common deterrent.
- Prior experience: Veterinarians often rely on their past experience with pyometra cases.
- Poor owner compliance: Owners may decline additional testing due to financial or other reasons. Veterinarians in specialty practice reported significantly more owner refusals for culture submission. This suggests a potential gap in owner education regarding the value of this diagnostic tool, or possibly the increased cost associated with specialty care.
- Result turnaround time: Culture results can take several days, delaying targeted treatment.
- Anticipated results: Many veterinarians assume E. coli is the causative agent, leading to empiric treatment without confirming the specific bacterial strain or its antibiotic sensitivities.
Why Culture is Essential for Effective Pyometra Antibiotics
While E. coli is indeed the most common bacterium isolated from pyometra cases, assuming its presence and susceptibility without testing can be problematic. Bacterial culture and sensitivity testing are crucial because they:
- Identify the specific bacteria: Confirming the exact organism causing the infection.
- Determine antibiotic sensitivity: Showing which antibiotics will be effective against that specific bacterial strain and which ones will not. This allows for targeted, effective treatment, avoiding the use of ineffective drugs and minimizing broad-spectrum antibiotic exposure.
- Help combat resistance: By identifying resistant strains, veterinarians can avoid contributing to the problem by using drugs that won’t work, thereby guiding the selection of appropriate pyometra antibiotics. Without cultures, resistance patterns within a population cannot be accurately determined.
The original study also noted differences in sample collection methods between general and specialty practices, with general practitioners more likely to use purulent fluid samples and specialty practitioners more likely to use wall swabs. The ideal tissue sample for accurate assessment of secondary infection in pyometra remains an area requiring further research.
Bridging the Gap: Alternatives and Education
In situations where a full culture isn’t feasible, alternatives like Gram staining (a point-of-care test) can offer immediate insights into the likely type of bacteria present. However, for definitive sensitivity, laboratory culture remains the gold standard. For severely affected pyometra cases, especially those with signs of systemic inflammatory response syndrome (SIRS) or sepsis, early empiric antibiotic use is often necessary while awaiting culture results. Once results are available, the antibiotic choice can be “de-escalated” to a narrower, more targeted spectrum.
To improve the judicious use of pyometra antibiotics, there’s a clear need to:
- Decrease the cost of culture.
- Improve turnaround times for results.
- Enhance client education about the significant value of culture testing.
Understanding Antibiotic Duration and Effectiveness
The study highlighted a significant lack of consensus on the ideal duration for postoperative pyometra antibiotics. While some studies report durations ranging from 5 to 53 days, the Arizona survey revealed that many practitioners chose durations arbitrarily, from 2 to 30 days.
For comparison, in human medicine, for “clean” surgical procedures, perioperative antibiotics are often concluded within 24 hours. Prolonged antibiotic administration, especially when unnecessary, has been strongly linked to the development of antimicrobial resistance. While an uncomplicated ovariohysterectomy is a clean procedure, pyometra cases can be more complex due to systemic illness, which may warrant some antibiotic coverage. However, the exact need and optimal duration of extended postoperative therapy for dogs with pyometra are still poorly understood. This underscores the need for more research to establish clear guidelines. Responsible pet ownership also includes seeking professional advice regarding conditions like pyometra and considering options for prevention and care for your dog. For example, understanding how to manage parasites can prevent other health issues; learning about chewable flea and tick meds for dogs is part of comprehensive care.
Escherichia coli, the most common culprit in pyometra, is known to have varied resistance patterns and is intrinsically resistant to certain antibiotics like clindamycin, erythromycin, and penicillin. This knowledge is crucial when a veterinarian chooses empiric therapy (treatment before culture results are known), as selecting an ineffective antibiotic can delay recovery and contribute to resistance.
When Are Antibiotics Most Crucial? Triggers and Clinical Signs
The survey asked veterinarians about factors that trigger their decision to use postoperative pyometra antibiotics. These triggers are essential for identifying cases where antibiotic intervention is most critical.
General Triggers for Postoperative Antibiotic Use
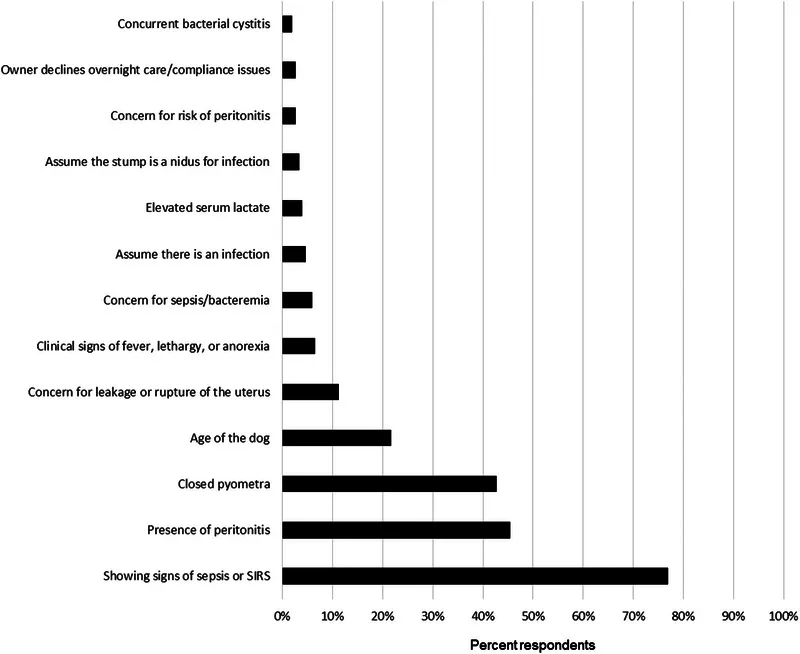 Veterinarian reported triggers for initiating postoperative pyometra antibiotics in dogs, such as systemic illness or surgical complications
Veterinarian reported triggers for initiating postoperative pyometra antibiotics in dogs, such as systemic illness or surgical complications
The most frequently reported triggers included signs of systemic illness, intraoperative complications (e.g., uterine rupture, peritoneal contamination), and ongoing inflammation.
Physiologic Parameters and Clinical Signs
Specific physiological parameters and clinical signs also played a significant role in encouraging antibiotic use:
 Physiologic and blood work parameters that influence veterinarians’ decisions to prescribe pyometra antibiotics, including fever and white blood cell count changes
Physiologic and blood work parameters that influence veterinarians’ decisions to prescribe pyometra antibiotics, including fever and white blood cell count changes
These included:
- Changes in body temperature: Fever or hyperthermia (high temperature) was a trigger for 27% of respondents. Febrile pyometra cases have a three times higher risk of developing peritonitis, suggesting the importance of early antibiotics.
- Changes in heart rate and respiratory rate: These are key indicators of systemic distress and potential SIRS.
- White blood cell count changes: Leukopenia (low white blood cell count) or leukocytosis (high white blood cell count) were reported as triggers by 22% of respondents. Leukopenia, in particular, has been identified as a prognostic indicator in pyometra, often associated with longer hospital stays and peritonitis.
- Hypotension (low blood pressure): Although reported by some, it was not a universal trigger.
These signs are defining characteristics of Systemic Inflammatory Response Syndrome (SIRS) and sepsis, which are severe, life-threatening conditions requiring aggressive treatment, including prompt administration of pyometra antibiotics. The prevalence of SIRS in pyometra cases can be as high as 57-61%, often linked to endotoxin release from E. coli. For comprehensive care, it’s also important to consider all aspects of your dog’s health, including protection against various diseases. For instance, understanding heartworm medicine for dogs is another vital part of preventative health.
Addressing Antibiotic Resistance: A Shared Responsibility
The problem of antimicrobial resistance is not confined to human medicine; it is a global health challenge affecting both humans and animals. Multidrug-resistant infections in animals can contribute to resistance in humans, underscoring the interconnectedness of “One Health.” The high percentage of veterinarians routinely using pyometra antibiotics and the low rate of culture submission in the survey population raise concerns about potential overuse. While a direct conclusion of “overuse” cannot be drawn without detailed patient-specific clinical data, the patterns suggest a need for greater awareness and more judicious practices.
What Dog Owners Can Do
As a responsible dog owner, you have a role in combating antibiotic resistance:
- Be informed: Understand your dog’s condition and the rationale behind your vet’s treatment recommendations, including antibiotic use.
- Ask questions: Don’t hesitate to ask your veterinarian about bacterial culture, the specific antibiotic prescribed, its dosage, and the expected duration of treatment.
- Adhere strictly to instructions: Always administer antibiotics exactly as prescribed by your vet, completing the full course even if your dog seems to be feeling better. Stopping early can lead to incomplete eradication of bacteria and foster resistance.
- Discuss alternatives: If appropriate for your dog’s specific case, discuss with your vet whether ovariohysterectomy alone might be sufficient without prolonged antibiotics for less severely affected pyometra cases.
Veterinary Stewardship
Veterinarians play a pivotal role in antibiotic stewardship. The goal is to institute educated empiric antibiotic use, encourage regular culture submission (especially in severe or atypical cases), and determine appropriate treatment types, doses, and durations. This approach improves the quality of care for canine patients while actively reducing the risk of resistance. For more information on preventative care, explore options like best treatment to prevent ticks on dogs to protect your pet from other common health threats.
Towards Better Guidelines for Pyometra Antibiotics
The findings of this survey underscore a clear and urgent need for the development of specific, evidence-based guidelines for the use of bacterial culture and pyometra antibiotics following ovariohysterectomy in dogs. Without such guidelines, treatment practices will continue to vary, potentially contributing to the growing challenge of antimicrobial resistance.
Future prospective clinical studies are essential to:
- Determine the ideal antibiotic selection based on different clinical scenarios.
- Establish appropriate doses and durations of antibiotic therapy.
- Compare outcomes of pyometra cases treated with and without postoperative antibiotics.
- Investigate the cost-effectiveness and accessibility of culture and sensitivity testing.
By actively participating in informed discussions with your veterinarian and advocating for judicious antibiotic use, dog owners can contribute to better health outcomes for their pets and help preserve the effectiveness of these vital medications for the future. Understanding all aspects of pet health, from serious conditions like pyometra to everyday parasite prevention with flea tick meds for dogs, empowers you to make the best decisions for your cherished companion.
Conclusion
Pyometra is a critical condition requiring prompt and effective veterinary care. While surgery remains the cornerstone of treatment, the role of pyometra antibiotics is a nuanced one. The recent survey highlighted the variability in antibiotic use among veterinarians and the low rate of bacterial culture submission, indicating a significant need for clearer, evidence-based guidelines. The rise of antimicrobial resistance makes it more imperative than ever to use antibiotics judiciously, ensuring they are prescribed only when necessary and in the most effective manner possible.
As dog owners, our best defense is knowledge and proactive communication with our veterinarians. By understanding the complexities of pyometra, the importance of bacterial culture, and the global challenge of antibiotic resistance, we can work together with our vets to ensure our beloved dogs receive the highest standard of care while safeguarding the future efficacy of antibiotics. Always complete the full course of prescribed medication and never hesitate to ask questions about your dog’s treatment plan.
References
- Lavin, L. E., & Maki, L. C. (2023). Antimicrobial use in the surgical treatment of canine pyometra: A questionnaire survey of Arizona‐licensed veterinarians. Veterinary Medicine and Science, 9, 1124–1133. 10.1002/vms3.1130
- Agostinho, B. P., Oliveira, M. C., Santana, P. C., Silva, D. R., Silva, D. F., Ferreira, D. O., de Menezes, V. D. C., & Azevedo, C. S. (2014). Canine pyometra: analysis of clinical, haematological, biochemical and cytological findings in 18 cases. Journal of Veterinary Medical Science, 76(12), 1625-1630.
- Bratzler, D. W., & Houck, E. A. (2005). Antimicrobial prophylaxis in surgery. Archives of Surgery, 140(2), 174-182.
- Fieni, F., Lejeune, A., Dumon, C., et al. (2014). Canine pyometra: an update on medical management. Reproduction in Domestic Animals, 49 Suppl 2, 19-24.
- Fransson, B. (2012). Canine pyometra: a review. Veterinary Clinics of North America: Small Animal Practice, 42(3), 513-524.
- Hagman, R. (2022). Canine pyometra: a review on current treatment and management. Veterinary Medicine and Science, 8(1), 1-13.
- Jitpean, S., Hagman, R., Wernersson, S., et al. (2017). Outcome of pyometra in dogs: A cohort study. Journal of Small Animal Practice, 58(11), 609-614.
- Weese, J. S., Giguère, S., Guardabassi, L., et al. (2015). ACVIM consensus statement on antimicrobial stewardship in veterinary medicine. Journal of Veterinary Internal Medicine, 29(4), 1162-1172.
