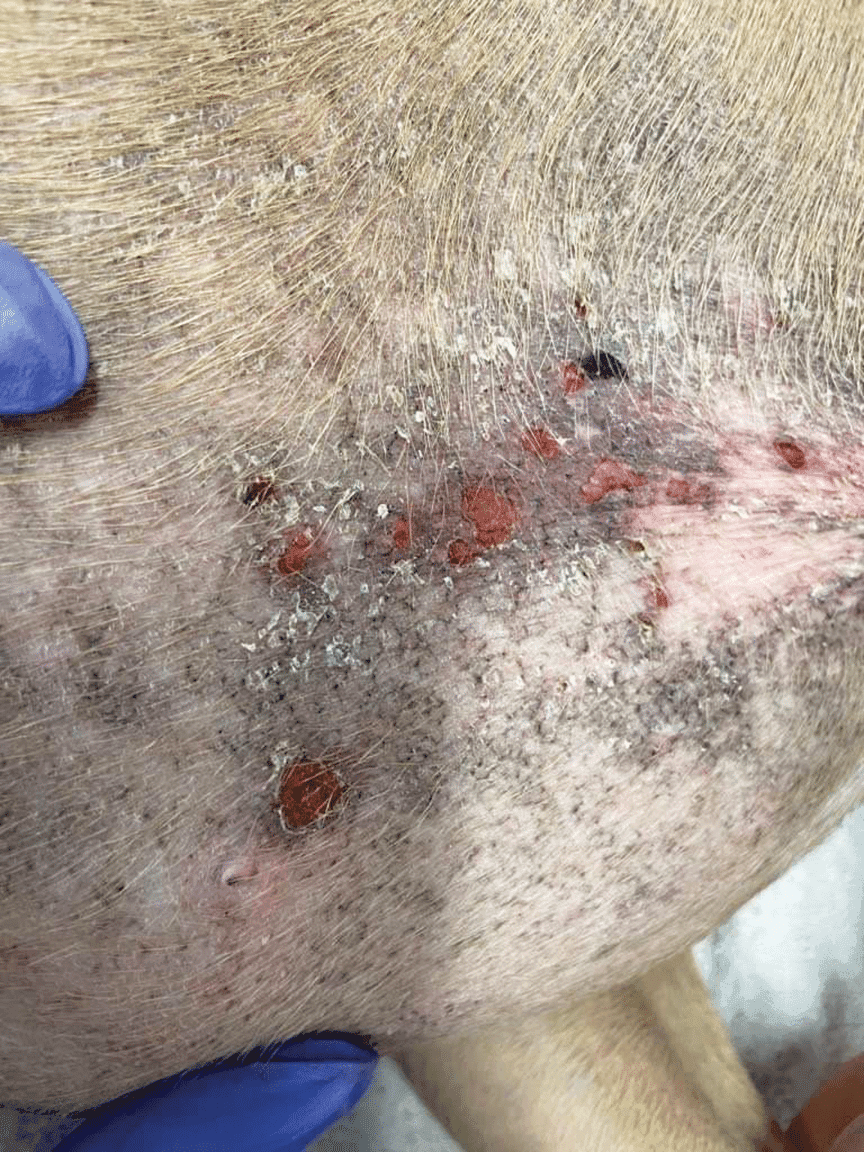
When your dog’s immune system, designed to protect them from external threats, mistakenly attacks their own body, it can lead to a range of health issues. One of the more distressing manifestations of these autoimmune disorders is spontaneous, nasty skin lesions. These eruptions can cause significant pain and discomfort for your canine companion, often stemming from the immune system’s misguided assault on the outer epidermis and inner dermis.
As these crucial skin layers separate, the formation of painful blisters and pustules becomes common. These delicate structures are prone to erosion, leading to crusting from the discharge of fluids and debris, and ultimately resulting in hair loss in the affected areas. Secondary bacterial infections frequently complicate these autoimmune skin conditions, necessitating prompt veterinary attention. While the exact triggers for autoimmune skin diseases in dogs are not always clear, recurring severe atopic dermatitis is often a suspected precursor, predisposing dogs to these more complex autoimmune issues. Symptoms associated with atopy can include persistent itching, sneezing, skin rashes, watery eyes, and excessive paw chewing. Unfortunately, by the time a definitive diagnosis is made, the initial trigger may have long since passed, making the diagnostic and treatment process challenging.
While viruses are known triggers for autoimmune skin conditions in humans, their role in dogs is less documented. Though a genetic predisposition is recognized in human autoimmune disorders, it has not been definitively proven in dogs, but it is strongly suspected. Some breeds, like the Akita, are recognized as being more frequently affected by conditions such as superficial pemphigus. Certain medications, including antibiotics like sulfonamide, penicillin, and cephalosporin, can also act as triggers in individual dogs. Similarly, topical medications used for external parasite control, such as those containing fipronil, amitraz, S-methoprene, dinotefuran, pyriproxyfen, or permethrin, have been implicated. In cases where a medication is the culprit, discontinuing the drug may lead to the restoration of normal skin, while other dogs will require ongoing treatment to manage and maintain skin health.
Diagnosis of Autoimmune Skin Diseases
Autoimmune skin diseases in dogs, while not exceedingly common, do occur and require a careful diagnostic approach. A comprehensive medical history is crucial to rule out any potential drug-induced conditions, and parasitic causes for the skin lesions must also be eliminated. If these initial investigations do not yield a clear answer, a skin biopsy becomes the definitive method for diagnosing an autoimmune skin problem.
However, obtaining an accurate biopsy can be complicated. Ideally, the biopsy should capture a vesicle or pustule before it erodes, but these lesions are exceptionally fragile and rarely found intact in time for sampling. Furthermore, any prior treatment can significantly skew the biopsy results, potentially leading to an incorrect diagnosis. As experienced veterinarians note, confirming an autoimmune skin disease often necessitates a biopsy, even with extensive experience.
The cost associated with biopsies can be a barrier, leading veterinarians to sometimes opt for a therapeutic trial with steroids first. If steroids do not provide adequate relief, or if the lesions recur after stopping the medication, a biopsy may then be pursued. A significant challenge with this approach is the requirement to cease steroid use for 14 to 21 days before the biopsy can be taken, as continued steroid use will alter the histological findings.
Treatment Strategies for Canine Autoimmune Skin Disease
Effective treatment for autoimmune skin diseases in dogs often involves a combination of medications to achieve faster results and reduce the risk of side effects from individual drugs at higher doses. Typical treatment protocols begin with glucocorticoids, such as prednisone, administered alone or in conjunction with potent immunosuppressive medications like azathioprine or cyclosporine.
Steroids are generally affordable and easy for owners to administer at home. However, their long-term use can lead to significant side effects, including increased thirst and urination, and potentially escalating to serious conditions such as diabetes mellitus, liver disease, and Cushing’s disease. Pulse therapy, involving intermittent administration of high doses, may be recommended, especially when dogs initially receive high steroid doses, followed by periodic dosing rather than daily lower doses. For milder or localized issues, topical steroids or immunomodulators, like tacrolimus, might be sufficient to maintain remission.
Antibiotics are frequently necessary to address secondary bacterial infections that can flourish on compromised skin. A culture and sensitivity test is recommended to identify the most effective antibiotic. Dogs suffering from atopy or other allergic dermatitis conditions will benefit from concurrent treatment of these underlying issues, as well as any secondary yeast or fungal infections.
Emerging therapeutic avenues for canine autoimmune skin disease include acupuncture, often integrated with herbal remedies such as radix Curcuma wenyujin, Tripterygium wilfordii, Artemisia annua, and Berberis vulgaris. Oclacitinib (Apoquel) has shown promise, though further research is needed for widespread recommendation. A notable advantage of oclacitinib is its generally lower incidence of significant side effects and improved safety profile compared to long-term corticosteroids.
Some dogs may experience periods of remission, allowing for weaning to low medication levels or even temporary cessation of medication. However, recurrence of the disease is common in most instances. It is also advisable to avoid frequent shampooing during active flare-ups. Shampoos, particularly those containing lower concentrations of hydrocortisone, may not be potent enough, and the mechanical action of bathing and rinsing can exacerbate the fragility of already compromised autoimmune skin, potentially worsening the condition. For dogs experiencing diarrhea, seeking advice on anti diarrhea meds for dogs or exploring otc for dog diarrhea can be part of a supportive care plan, though these should always be discussed with a veterinarian, especially in the context of underlying autoimmune issues. Given the complexity of skin conditions, ensuring your dog is protected against external parasites is also vital, and researching best flea and tick meds for large dogs or best dog flea treatment without vet prescription can be considered as part of overall health management.
This article was reprinted with permission from the Cornell University College of Veterinary Medicine’s DogWatch newsletter.