Dermatophytic pseudomycetoma (DPM) in cats is a rare, deep dermal and subcutaneous fungal infection primarily caused by dermatophytes like Microsporum canis. Unlike common superficial ringworm infections, DPM penetrates deeper tissues, leading to severe nodules, ulcers, and grains of fungal material. This condition has been mostly reported in Persian cats, but cases in other breeds, such as domestic short-haired cats, highlight its potential in any feline. For cat owners, recognizing early signs like persistent crusts, nodules, and itching is crucial, as delayed treatment can lead to systemic complications. This article details a real-world case of DPM in a 3-year-old spayed female Korean Short Hair Cat, exploring diagnosis, treatment challenges, and outcomes to help pet guardians understand this uncommon but serious skin issue.
Case Presentation
The patient was a 3-year-old indoor female domestic Korean Short Hair cat weighing 3 kg. She presented with a one-year history of skin crusts, nodules, pruritus (itching), and weight loss. Symptoms began with crusts on the nasal bridge, progressing to widespread lesions across the body. Three months prior to advanced care, a local vet diagnosed dermatophytosis via fungal culture and treated her with two doses of an inactivated M. canis vaccine (Biocan M) and oral itraconazole. However, lesions persisted and worsened, with new multifocal nodules appearing. Notably, she lived with 13 other cats, none of which showed symptoms, suggesting individual susceptibility rather than environmental spread.
At presentation, physical exams revealed multifocal ulcerative nodules on the ventral thorax, abdomen, flank, and left hindlimb, covered in yellowish grains. These grains are micro-aggregates of the fungus, a hallmark of DPM.
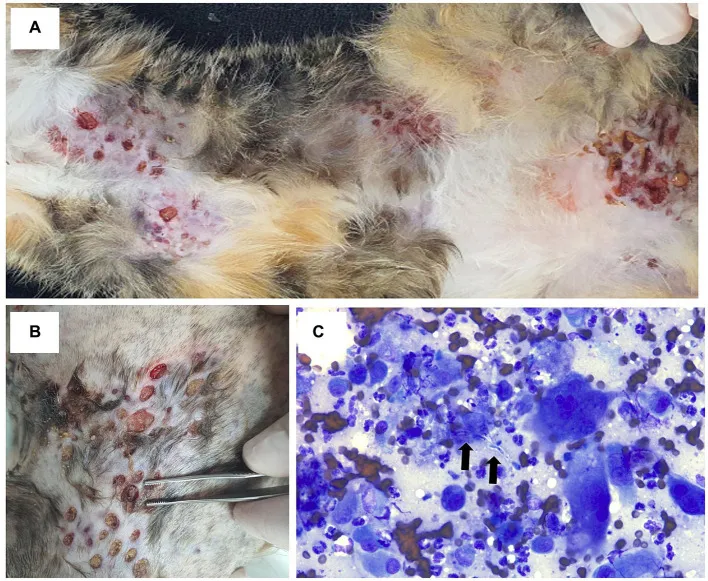 Multifocal ulcerated nodules on the cat's thorax, abdomen, flank, and limbs with serosanguinous discharge and yellowish grains on the surface
Multifocal ulcerated nodules on the cat's thorax, abdomen, flank, and limbs with serosanguinous discharge and yellowish grains on the surface
Cytology from fine-needle aspiration of the nodules showed degenerative neutrophils, macrophages, multinucleated giant cells, and fungal hyphae, confirming active fungal elements amid inflammation.
Diagnostic Assessment
Diagnostic workup included cytology, histopathology, cultures, and systemic evaluations. Bacterial culture on blood agar identified Staphylococcus aureus, indicating secondary pyoderma. Fungal culture on Sabouraud agar confirmed Microsporum canis. Histopathology from 6 mm punch biopsies revealed pyogranulomatous dermatitis with fungal plaques—irregular hyphae showing bulbous or spore-like dilatations centered in inflammatory nodules.
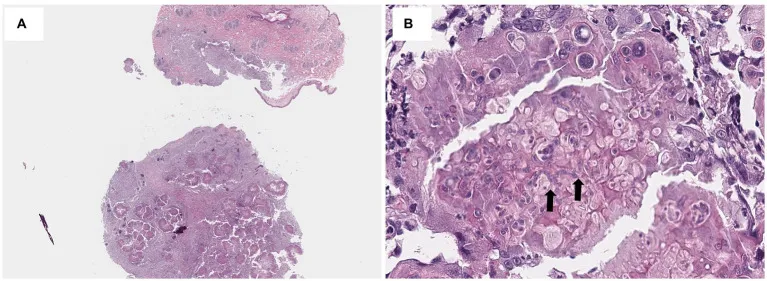 Histopathological view of dermis expanded by nodular inflammatory infiltrate with macrophages, neutrophils, lymphocytes, plasma cells, and central irregular fungal hyphae (H&E staining, 40x and 400x)
Histopathological view of dermis expanded by nodular inflammatory infiltrate with macrophages, neutrophils, lymphocytes, plasma cells, and central irregular fungal hyphae (H&E staining, 40x and 400x)
Bloodwork showed leukocytosis, hypoalbuminemia, elevated liver enzymes (ALT, AST), total bilirubin, amylase, hyperglycemia, hyperglobulinemia, and high feline serum amyloid A—markers of inflammation and stress. However, thyroid (T4), FeLV/FIV tests, anemia PCR panel, and imaging (abdominal ultrasound, radiographs) were normal or negative. Elevated enzymes were attributed to prior antifungals, not primary disease.
The diagnosis: DPM due to M. canis with secondary bacterial infection. No underlying immunodeficiency was identified, though genetic or immune factors may play a role, as seen in Persian predispositions.
Treatment Interventions
Initial therapy included oral itraconazole (10 mg/kg once daily), cephalexin (20 mg/kg twice daily for pyoderma), chlorhexidine wipes, and ketoconazole ointment. After four weeks, pruritus lessened, but nodules persisted and new ones emerged on the abdomen.
Surgery was declined by the owner, prompting alternative approaches. Intralesional (IL) amphotericin B was selected for its efficacy in deep fungal nodules (e.g., sporotrichosis). Under dexmedetomidine sedation, amphotericin B (1 mg/mL dilution) was injected at 0.6 mg per nodule across 17 sites (total 3.4 mg/kg body weight), followed by saline infusion. Three weekly injections were given, combined with oral terbinafine (30 mg/kg twice daily) for synergy.
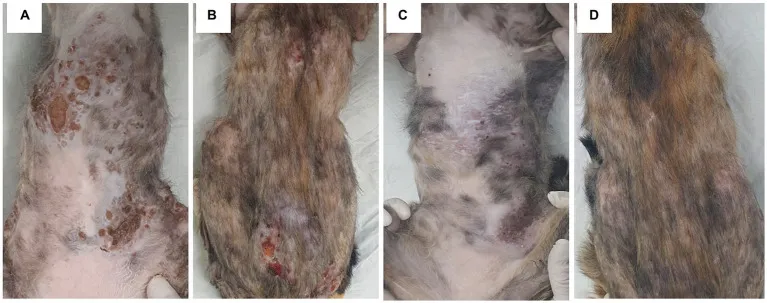 Skin lesion progression: initial multiple large ulcerative nodules on thorax, abdomen, and trunk (A,B); after three IL amphotericin B injections and oral terbinafine, reduced ulceration and nodule count, though large dome-shaped nodules persisted (C,D)
Skin lesion progression: initial multiple large ulcerative nodules on thorax, abdomen, and trunk (A,B); after three IL amphotericin B injections and oral terbinafine, reduced ulceration and nodule count, though large dome-shaped nodules persisted (C,D)
Post-treatment (four weeks): Ulceration resolved markedly, nodule number and size decreased, but large dome-shaped nodules remained refractory. Mild BUN elevation occurred post-amphotericin but normalized. Additional three IL injections on remaining nodules yielded no further improvement. Oral terbinafine and itraconazole continued for five months, stabilizing lesions.
Outcomes and Follow-Up
Nine months post-presentation, multifocal ulcerative nodules recurred with anemia, leukocytosis, worsened liver enzymes, bilirubin, and hyperglobulinemia. Despite antifungals, fluids, transfusion, and tube feeding, the cat’s condition deteriorated, leading to death at 10 months.
IL amphotericin B and terbinafine offered partial success—reducing ulceration and smaller nodules—but failed against large lesions. Recurrence underscores DPM’s aggressiveness.
Discussion on DPM Management in Cats
DPM arises from dermatophyte invasion beyond follicles into dermis/subcutis, forming granulomatous reactions with grains. Rare in short-haired breeds, this case suggests superficial dermatophytosis progression without clear predisposition. Standard treatments (griseofulvin, azoles) often fail; surgery plus prolonged antifungals shows better results in Persians.
Amphotericin B’s IL use leverages high local concentrations with minimal systemic risks, proven in other mycoses. Here, lower per-nodule dosing (to cap total body weight dose) may explain incomplete response versus prior reports. Terbinafine inhibits ergosterol synthesis effectively against dermatophytes, with mixed DPM outcomes. Combination therapy stabilized but didn’t cure, highlighting needs for optimized protocols, higher targeted doses on large nodules, and surgery.
Relapses indicate subclinical spread or immune factors. Owners should monitor for crusts/alopecia, seek prompt fungal cultures/histology, and consider vet specialists. Prognosis improves with early intervention.
In summary, DPM demands multimodal therapy; IL amphotericin B plus oral terbinafine is a viable option for refractory cases, though further dosing studies are needed. Cat owners facing persistent skin nodules should consult a veterinary dermatologist immediately for cultures and biopsies—early action can prevent progression.
References
- Feline dermatophytic pseudomycetoma reports.
- Microsporum canis in deep infections.
- Persian cat predisposition studies.
4-6. Antifungal trials (griseofulvin, ketoconazole, terbinafine, itraconazole).
7-12. Amphotericin B applications in fungal diseases.
For more on cat skin health, explore our guides on ringworm prevention and when to see a vet. Always prioritize professional veterinary advice tailored to your pet.
