When you take your beloved canine companion for their annual veterinary check-up, you might wonder why your vet suggests a screening blood panel and urinalysis, especially if your dog seems perfectly healthy. This proactive approach allows your veterinarian to uncover the early onset of conditions that haven’t yet manifested with obvious signs. Chronic kidney disease (CKD) in dogs is a prime example of such a condition, often progressing silently before symptoms become apparent. Understanding the role of Kidney Medicine For Dogs and early intervention is critical for maintaining your pet’s comfort and well-being.
Acute (sudden onset) kidney disease typically presents with clear and immediate signs of illness. However, chronic kidney disease develops gradually over time, and its initial signs and symptoms can be subtle, easily overlooked, or attributed to normal aging. Early diagnosis and timely intervention are paramount to effectively managing the disease, slowing its progression, and ensuring the best possible quality of life for your dog. Your veterinarian’s recommendations, including potential kidney medicine for dogs, are tailored to address the specific stage and needs of your pet, making routine screenings an invaluable part of preventative care.
Key Takeaways
- Kidney disease can be present long before pet parents notice obvious symptoms.
- Early signs often include increased thirst and urination, lethargy, a picky appetite, or weight loss—symptoms that can also point to many other conditions, underscoring the need for veterinary assessment.
- Blood work and urinalysis are fundamental diagnostic tests for canine kidney disease, but further diagnostics may be necessary for a complete picture.
- Chronic kidney disease is generally not curable and is progressive, but it can be effectively managed with appropriate kidney medicine for dogs, dietary changes, and supportive care to significantly improve a dog’s quality of life.
Understanding Chronic Kidney Disease (CKD) in Dogs
Dogs possess two kidneys, organs absolutely vital for maintaining numerous day-to-day life processes. Their primary function is to filter waste products and toxins from the bloodstream and excrete them from the body through urine. Beyond filtration, the kidneys perform several other critical tasks: they regulate fluid, mineral, and electrolyte balance; conserve essential water and certain blood proteins; help maintain healthy blood pressure; and are involved in the production of red blood cells.
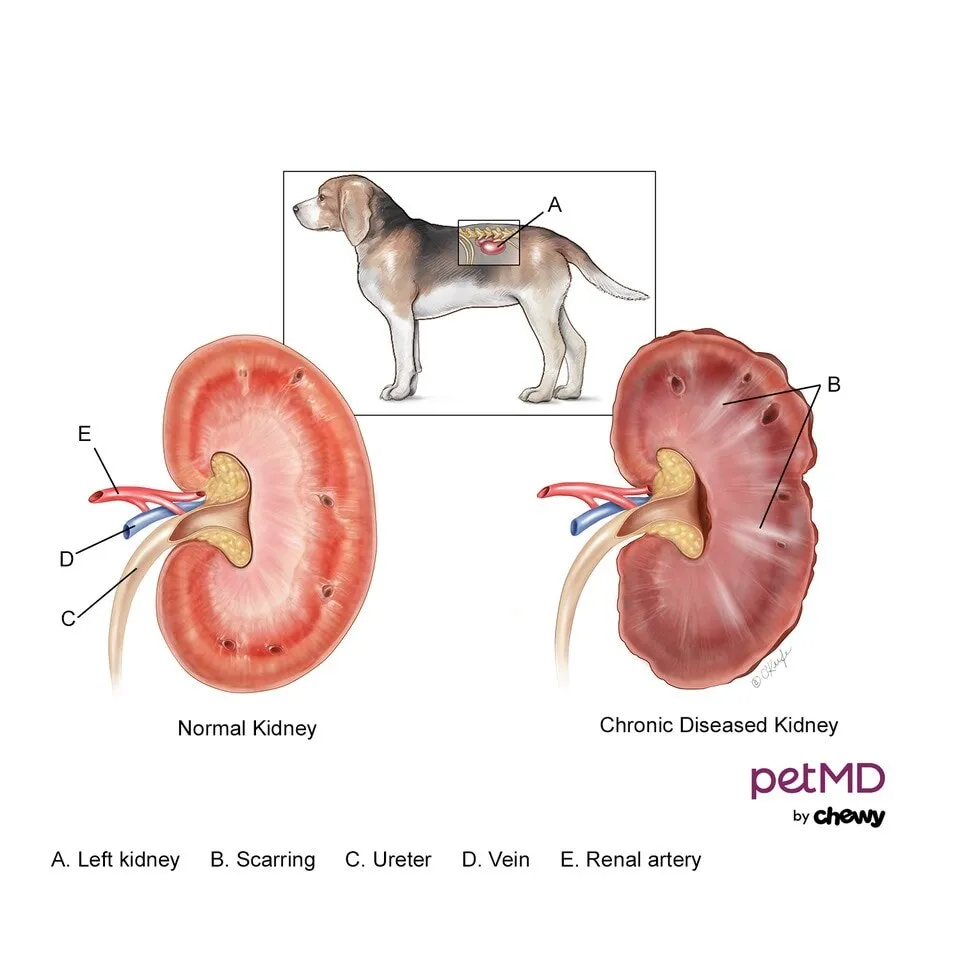 Diagram illustrating the differences between a healthy dog kidney and a kidney affected by chronic disease, explaining kidney function and damage
Diagram illustrating the differences between a healthy dog kidney and a kidney affected by chronic disease, explaining kidney function and damage
Many factors can contribute to the progressive loss of kidney function. Unfortunately, once kidney damage occurs, it is largely irreversible. As kidney function declines, unfiltered waste products and toxins accumulate in the bloodstream, leading to a generalized state of discomfort, nausea, and malaise, a condition known as uremia. When left untreated or inadequately managed, a dog’s overall quality of life suffers dramatically.
Chronic kidney disease (CKD) in dogs is by definition a progressive condition that often goes unnoticed for an extended period before a diagnosis is made. Its progression rate varies uniquely for each patient, making it challenging to predict. Veterinarians typically classify CKD into four stages (IRIS stages I–IV) based on specific laboratory values and observable clinical signs or symptoms. This staging helps guide the selection of appropriate kidney medicine for dogs and other therapeutic strategies.
Recognizing Symptoms of CKD in Dogs
A significant challenge with CKD is that dogs usually do not exhibit noticeable symptoms until approximately 75% of their kidney functioning capacity has been lost. This delay highlights why early detection through routine veterinary screenings is so crucial. The higher the IRIS stage, the more pronounced and numerous the symptoms typically become, and they may worsen in severity and complexity as the disease advances.
Symptoms of kidney failure in dogs are varied and can include:
- Anemia (a reduced red blood cell count), often a secondary complication of advanced CKD.
- Changes in urine output, most commonly an increase in the frequency and volume of urination.
- Decreased appetite, leading to reluctance to eat or complete meals.
- Dehydration, despite increased water intake, due to the kidneys’ inability to conserve water.
- Increased thirst, as the body attempts to compensate for fluid loss.
- Muscle wasting, particularly noticeable over the back and hips, contributing to weight loss.
- Nausea, which may manifest as lip-licking or drooling.
- Oral ulcerations (sores in the mouth) and noticeably bad breath (halitosis) due to uremic toxins.
- Pale gums, a sign of anemia.
- Poor coat appearance, which may be dull, dry, or unkempt.
- Sporadic vomiting, often worsening as the disease progresses.
- Vision loss, sometimes linked to secondary hypertension (high blood pressure).
- Weakness and lethargy, causing reduced activity levels.
- Weight loss, even if the dog is still eating.
If you observe any of these signs, particularly a combination of them, it’s imperative to consult your veterinarian immediately to discuss potential diagnostic steps and the appropriate course of action, which may include starting kidney medicine for dogs. While discussing health issues with your vet, you might also ask about general preventative care such as flea tick and lice treatment for dogs, as overall health can impact kidney function.
Common Causes and Risk Factors for Canine Kidney Disease
Chronic renal failure is, by definition, a disease that develops over an extended period. It represents an ongoing, progressive, and irreversible process. For many dogs, the precise cause of their CKD may remain unknown even after extensive diagnostic testing.
Sometimes, chronic kidney disease in dogs can develop as a long-term consequence of a severe acute kidney injury. Such injuries can stem from:
- Serious infections: This includes conditions like leptospirosis, various tick-borne diseases, or pyelonephritis (a severe kidney infection).
- Environmental factors: Heatstroke can cause significant damage to multiple organs, including the kidneys.
- Toxin ingestion: Exposure to harmful substances such as antifreeze (ethylene glycol), certain over-the-counter NSAIDs like ibuprofen (which are toxic to dogs), or specific antibiotics can lead to kidney damage.
- Envenomation: Bites or stings from venomous creatures can also result in acute kidney injury that may progress to CKD.
Additionally, chronic kidney disease is sometimes associated with certain types of immune-mediated diseases, where the dog’s immune system mistakenly attacks its own kidney tissues, or with various forms of cancer that can directly affect kidney function or cause systemic changes detrimental to the kidneys. Beyond these factors, genetics also play a role, with certain dog breeds showing a higher predisposition to CKD, including:
- Bernese Mountain Dog
- Bull Terrier
- Cavalier King Charles Spaniel
- English Cocker Spaniel
- West Highland White Terrier
Understanding these potential causes is important, as addressing any underlying conditions can be a part of a comprehensive treatment plan that might involve specific kidney medicine for dogs to manage symptoms and slow disease progression. It’s also important for pet owners to be aware of other common dog health issues, such as the need for heartworm medicine for dogs, which is vital for preventative care and maintaining overall health.
Diagnosing Kidney Disease in Your Dog
The diagnostic process for chronic kidney disease typically begins with a thorough physical examination, accompanied by comprehensive blood work and a urinalysis. These foundational tests provide crucial insights into kidney function and overall health. Veterinarians will specifically evaluate several key values, including:
- Blood Urea Nitrogen (BUN): Elevated BUN levels are often correlated with reduced kidney function and failure.
- Calcium: While less common, elevated calcium levels can be observed as kidney disease progresses.
- Creatinine (Cr or Creat): This is a primary indicator of the kidneys’ efficiency in filtering waste products from the blood. Higher levels suggest impaired filtration.
- Electrolytes: Monitoring sodium, potassium, and chloride levels is essential, as kidney dysfunction can disrupt their balance.
- Phosphorus: Increased phosphorus levels are frequently associated with chronic kidney disease and require careful management.
- Red blood cell count: A low red blood cell count (anemia) is often a secondary complication seen in more severe stages of CKD due to reduced erythropoietin production by the kidneys.
- Symmetric Dimethylarginine (SDMA): SDMA is a more sensitive and early indicator of kidney disease, capable of detecting dysfunction earlier than creatinine.
- Urine Specific Gravity (USG): This measures the kidneys’ ability to concentrate urine. A lower USG indicates diluted urine, which can suggest impaired kidney function, as healthy kidneys should efficiently reabsorb water to prevent dehydration.
Beyond these basic tests, your veterinarian may recommend additional diagnostics for a more comprehensive assessment:
- A Urine Protein to Creatinine (UPC) ratio helps quantify the amount of protein being lost in the urine (proteinuria), which can be an indicator of kidney damage.
- A urine culture may be performed, as dogs with chronic kidney disease are more susceptible to developing urinary tract infections.
- A blood pressure evaluation is often crucial, as hypertension (high blood pressure) is a common comorbidity in dogs with CKD.
- Radiographs (X-rays) or an abdominal ultrasound can screen for structural abnormalities such as kidney stones, tumors, or infarcts (areas of dead tissue within the kidney).
- In very rare and complex cases, a kidney biopsy may be considered to obtain a definitive diagnosis or characterize the specific type of kidney disease.
Comprehensive Treatment for Canine Kidney Disease
Chronic kidney disease in dogs is a manageable yet incurable condition. By the time symptoms become evident, irreversible damage to the kidney tissue has already occurred. The goal of treatment, which heavily relies on specific kidney medicine for dogs, is to slow the progression of the disease, alleviate symptoms, and maintain the best possible quality of life for your pet.
Treatment recommendations are highly individualized and tailored to match your dog’s specific needs based on the IRIS stage of their CKD. Dogs in Stages III or IV typically require more intensive care and a broader range of therapies compared to those in Stages I or II. Common therapeutic approaches for chronic kidney disease often combine medications, dietary management, and fluid therapy, alongside addressing any identified underlying conditions or inciting factors.
Medications for Symptom Management
A significant component of kidney medicine for dogs focuses on managing the clinical signs that arise from toxin accumulation. These include:
- Anti-nausea and anti-emetic medications: Drugs such as Cerenia (maropitant citrate), ondansetron, or proton pump inhibitors like omeprazole can effectively help treat nausea, vomiting, and a corresponding lack or loss of appetite. If your dog is throwing up, these medications are vital. For more generalized issues, you might consult about dog medicine for throwing up.
- Appetite stimulants: Medications like capromorelin (Entyce) and mirtazapine may be prescribed to encourage eating and combat weight loss, which is crucial for maintaining strength and energy.
- Phosphate binders: These oral medications are given with food to bind excess phosphorus in the gastrointestinal tract, preventing its absorption and reducing blood phosphorus levels, which are often elevated in CKD.
- Blood pressure medications: If hypertension is diagnosed, specific antihypertensive drugs like ACE inhibitors (e.g., benazepril) or calcium channel blockers (e.g., amlodipine) may be used to protect the kidneys and other organs.
- Anemia management: For dogs with significant anemia, iron supplements or erythropoiesis-stimulating agents (ESAs) might be considered to boost red blood cell production.
- Potassium supplements: Some dogs with CKD may develop hypokalemia (low potassium), requiring supplementation.
Dietary Management
Most veterinarians will strongly recommend a prescription renal diet as a cornerstone of managing CKD. These specialized diets are formulated to be:
- Lower in protein: Reduced protein levels help decrease the workload on the kidneys and minimize the production of nitrogenous waste products.
- Lower in phosphorus: This helps control elevated phosphorus levels, which can worsen kidney disease.
- Lower in sodium: Reduced sodium helps manage blood pressure and fluid retention.
- Alkalinized: These diets often help combat metabolic acidosis, a common side effect of CKD.
- Enriched with Omega-3 fatty acids: These can help reduce inflammation in the kidneys.
Fluid Therapy
Fluid management is an essential aspect of care. Fluids may be administered to help flush out toxic waste substances from the bloodstream, combat dehydration, and improve overall hydration. They can be given intravenously (IV) in a hospital setting for more acute dehydration or severe illness, or subcutaneously (underneath the skin) at home by pet owners after proper training. Ensuring your dog always has access to fresh, clean water is critical; a water fountain can be an excellent addition to encourage regular drinking.
Addressing Underlying Issues
If an underlying cause for kidney damage (e.g., a treatable infection) is identified, targeted therapy for that condition will also be part of the overall strategy. This comprehensive approach ensures that all contributing factors are addressed to optimize the dog’s health.
Long-Term Management and Quality of Life
Chronic kidney disease is a serious, lifelong condition that demands ongoing care, diligent monitoring, and consistent adjustment of kidney medicine for dogs and other therapies as symptoms evolve. Dogs with CKD typically require more frequent veterinary visits and diagnostic testing than healthy pets. At all stages of the disease, continuously assessing the dog’s quality of life is paramount.
It is crucial to adhere strictly to your veterinarian’s recheck guidelines and to continue all prescribed medications and dietary recommendations. Many of these will be required for the remainder of your dog’s life. Regular communication with your vet about any changes in your dog’s behavior, appetite, or general well-being is vital for prompt adjustments to the treatment plan.
Depending on the individual circumstances and progression of the disease, various measures can help keep your dog comfortable and ensure a good quality of life for as long as possible. The same types of treatments and kidney medicine for dogs outlined in the treatment section are applicable for long-term management, often adjusted in dosage or combination. These might also include:
- Dietary supplements: Products such as Azodyl, a pre/probiotic, are sometimes used to help decrease the accumulation of uremic waste products in the bloodstream by leveraging intestinal bacteria.
- Ongoing anti-nausea and anti-vomiting medications: These can be prescribed on an as-needed basis for dogs who experience intermittent episodes of vomiting and lack of appetite, helping to maintain their comfort and encourage food intake.
- Pain management: If chronic pain (e.g., from arthritis, which can be exacerbated by reduced activity in CKD dogs) is a factor, appropriate pain relief medications may be incorporated.
While there are many claims about home remedies for dogs, it is crucial to emphasize that for a serious condition like kidney disease, all treatment and management strategies, including any supplements, must be discussed and approved by your veterinarian.
Chronic Kidney Disease in Dogs FAQs
How long can a dog live with kidney disease?
The lifespan of a dog with chronic kidney disease is highly variable because the disease’s progression differs greatly among individuals. While some dogs, particularly those diagnosed in early stages with proper veterinary care and diligent management, can live for several years, others may decline more rapidly and sadly require euthanasia shortly after diagnosis due to a poor quality of life. The effectiveness of kidney medicine for dogs and dietary management plays a significant role in extending and improving their lives.
How fast does kidney disease progress in dogs?
The progression rate of chronic kidney disease in dogs is unpredictable, potentially spanning weeks to years before symptoms become noticeable to pet owners. By the time clinical signs are observed, it’s generally estimated that approximately 75% of kidney function has already been lost, and the damage is irreversible. The rate of decline can be influenced by the underlying cause of the kidney disease, the dog’s overall health, and the stage at which the disease is diagnosed. Some dogs will experience a much faster decline than others.
Regular checkups and routine veterinary visits are vital for earlier detection of CKD. Catching the disease in its initial stages allows for earlier intervention with appropriate kidney medicine for dogs and dietary adjustments, which can significantly slow progression, alleviate symptoms, ensure your dog’s comfort, and ultimately contribute to a better overall quality of life. Even common issues like the need for tick removal medicine for dogs can be discussed during these routine vet visits, highlighting the importance of comprehensive care.
Conclusion
Navigating a diagnosis of chronic kidney disease in your dog can be a challenging experience, but with a clear understanding of the condition and a proactive approach, you can significantly impact your dog’s health and happiness. The key lies in early detection, understanding the critical role of specialized kidney medicine for dogs, and committing to a consistent management plan developed in close partnership with your veterinarian.
Remember that CKD is an incurable but manageable disease, and the goal of treatment is always to enhance your dog’s quality of life, slow disease progression, and minimize discomfort. By diligently following your vet’s recommendations regarding diet, medications for symptom management, and regular check-ups, you provide your furry friend with the best possible chance to live comfortably for as long as possible. Stay vigilant for any changes in your dog’s health, and always consult your veterinarian for expert advice tailored to your pet’s specific needs.
