High blood pressure, or hypertension, is a serious health concern that can affect dogs, often without obvious signs until significant damage has occurred. As a dedicated dog owner, understanding canine hypertension and the available treatments is crucial for your pet’s long-term health and quality of life. This guide, drawing from expert veterinary consensus, will demystify Dog High Blood Pressure Medication, helping you work effectively with your veterinarian to manage this condition.
Just like in humans, blood pressure in dogs is a measure of the force of blood against the walls of their arteries. When this pressure remains consistently too high, it can lead to severe health complications. While many factors can influence a dog’s blood pressure, persistent hypertension requires careful management, often involving medication, to prevent irreversible harm to vital organs. One class of medication commonly used to manage canine hypertension, especially when kidney issues are present, includes ACE inhibitors. For more insights into specific types of treatments, you might find information on ace medication for dogs helpful.
Understanding High Blood Pressure in Dogs
What is Canine Hypertension?
Canine hypertension is characterized by a sustained increase in systemic arterial blood pressure. It generally falls into one of three categories: situational, secondary, or idiopathic.
- Situational Hypertension: This occurs due to stress or anxiety during a veterinary visit, often referred to as “white coat hypertension.” It’s a temporary rise in blood pressure and typically doesn’t require medication, but it’s important for veterinarians to differentiate it from true pathological hypertension.
- Secondary Hypertension: The most common type, secondary hypertension, is caused by an underlying disease or condition. This includes chronic kidney disease (CKD), hyperadrenocorticism (Cushing’s disease), diabetes mellitus, and pheochromocytoma. Certain medications or toxins can also induce hypertension.
- Idiopathic Hypertension: This diagnosis is made when high blood pressure persists without any identifiable underlying cause, after thorough diagnostic work-up. It’s less common but does occur.
How is High Blood Pressure Diagnosed in Dogs?
Accurate blood pressure measurement is key to diagnosing hypertension. While direct arterial catheterization is the gold standard, non-invasive methods like Doppler and oscillometric devices are commonly used in clinical settings. To ensure reliable results, measurements should be taken in a quiet environment, with minimal restraint, and after the dog has acclimated for 5-10 minutes. Typically, the first reading is discarded, and an average of 5-7 consistent measurements is taken. Blood pressure values are then categorized based on the systolic blood pressure (SBP) and the risk of target organ damage (TOD):
- Normotensive (minimal TOD risk): SBP < 140 mm Hg
- Prehypertensive (low TOD risk): SBP 140-159 mm Hg
- Hypertensive (moderate TOD risk): SBP 160-179 mm Hg
- Severely Hypertensive (high TOD risk): SBP ≥ 180 mm Hg
Factors Influencing Blood Pressure in Dogs
Several factors can influence a dog’s blood pressure readings and overall predisposition to hypertension. Age, for instance, can lead to small increases in SBP over time, although this effect is not universally observed in all studies. Gender may also play a minor role, with some studies noting slight differences between intact males and neutered dogs. Breed variations are significant; certain breeds, particularly hounds like Greyhounds, tend to have higher baseline blood pressure readings than others, though this can often be attributed to situational anxiety rather than true hypertension. Obesity has been linked to increased blood pressure in some studies, but its direct impact can be complex and intertwined with underlying health conditions. Furthermore, factors such as the measurement method, operator experience, and the dog’s temperament all contribute to variability in readings, underscoring the importance of standardized protocols for consistent and accurate diagnosis.
The Dangers of Untreated High Blood Pressure: Target Organ Damage (TOD)
The primary concern with sustained high blood pressure is its potential to cause damage to vital organs, known as Target Organ Damage (TOD). Preventing or minimizing this damage is the main goal of hypertension treatment. Organs most commonly affected include:
- Kidneys: Hypertension can accelerate the progression of chronic kidney disease (CKD) and induce proteinuria (excess protein in urine), which further damages the kidneys. Conversely, kidney disease can also cause hypertension.
- Eyes: Ocular lesions are frequently observed in hypertensive dogs. This can manifest as hypertensive retinopathy and choroidopathy, including retinal detachment, hemorrhage, edema, and even acute blindness.
- Brain: Hypertensive encephalopathy can lead to neurological signs such as lethargy, seizures, altered mental state, disorientation, balance disturbances, and even strokes.
- Heart and Blood Vessels: Persistent high blood pressure forces the heart to work harder, leading to left ventricular hypertrophy (thickening of the heart muscle). While less common, severe hypertension can lead to heart failure, epistaxis (nosebleeds), and rare but serious conditions like aortic aneurysm or dissection.
Identifying signs of TOD is a strong indicator for initiating antihypertensive treatment. Regular monitoring and diagnostic tests are crucial for detecting these issues early.
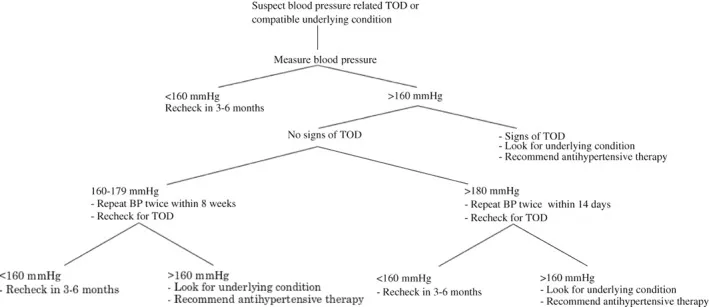 A flowchart showing the recommended approach to evaluating a possibly hypertensive dog, including blood pressure measurements and identification of target organ damage.
A flowchart showing the recommended approach to evaluating a possibly hypertensive dog, including blood pressure measurements and identification of target organ damage.
When Your Dog Needs Medication: Treatment Guidelines
Once hypertension is diagnosed and situational factors are ruled out, treatment typically involves a combination of managing the underlying cause and administering antihypertensive medications. Client education is paramount, as hypertension is often “silent,” meaning owners may not see immediate improvements in their dog’s well-being after starting medication. However, controlling blood pressure significantly improves long-term quality of life and reduces the risk of TOD.
General Principles of Hypertension Management
- Treat the Underlying Condition: Since hypertension in dogs is often secondary, addressing the primary disease (e.g., kidney disease, Cushing’s) is crucial. While treating the primary condition may help lower blood pressure, many dogs will still require specific antihypertensive drugs.
- Gradual Reduction: The goal is a gradual, persistent decrease in blood pressure, not an abrupt drop, which could lead to complications like hypoperfusion (insufficient blood flow).
- Individualized Treatment: Medication protocols are tailored to each dog, considering concurrent health conditions and individual responses.
- Monitoring and Adjustment: Frequent monitoring of blood pressure and overall health is necessary, especially during the initial phases of treatment, to ensure the medication is effective and to adjust dosages as needed. The ultimate goal is to reduce SBP to below 140 mm Hg or at least below 160 mm Hg.
- Owner Compliance: Regular discussions with your veterinarian about dosage, potential side effects, and follow-up appointments are vital for successful management. This approach helps ensure that treatments, such as those for conditions like pain medicine for dogs with hip dysplasia, are administered correctly alongside blood pressure medications.
Dietary Considerations
While dietary salt restriction is often suggested, current evidence indicates that substantial sodium restriction alone typically doesn’t significantly lower blood pressure in dogs. However, avoiding high dietary sodium chloride intake is generally recommended, as it may interact with certain antihypertensive medications and exacerbate conditions like kidney disease. The choice of diet should also account for other patient-specific factors, such as overall palatability and underlying or concurrent diseases. For dogs with chronic pain conditions, nutritional support can be as critical as specific medications, influencing overall treatment plans for issues like new arthritis medication for dogs.
Types of Dog High Blood Pressure Medication
The choice of medication for dogs with high blood pressure is largely guided by the underlying cause and the presence of any target organ damage. The most widely recommended antihypertensive agents for dogs are RAAS inhibitors and calcium channel blockers (CCBs).
RAAS Inhibitors (ACEi, ARB)
The Renin-Angiotensin-Aldosterone System (RAAS) plays a crucial role in regulating blood pressure. Inhibiting this system is a common first-line approach in dogs.
- Angiotensin-Converting Enzyme Inhibitors (ACEi): Drugs like enalapril or benazepril (typically 0.5-2.0 mg/kg orally every 12-24 hours) are frequently chosen, especially due to their antiproteinuric effect, which is beneficial for dogs with concurrent chronic kidney disease (CKD). They work by preferentially dilating the renal efferent arteriole, helping to reduce pressure within the kidney’s filtering units and thus decreasing proteinuria.
- Angiotensin Receptor Blockers (ARB): Telmisartan (e.g., 1.0 mg/kg orally every 24 hours) is an alternative RAAS inhibitor. While newer to veterinary use for hypertension, ARBs offer similar benefits to ACEi by blocking the effects of angiotensin II.
RAAS inhibitors should be used with caution in dehydrated dogs, as they can sometimes decrease glomerular filtration rate (GFR). Patients should be adequately rehydrated before starting these medications.
Calcium Channel Blockers (CCB)
- Amlodipine Besylate: This is a potent CCB and is often used in combination with RAAS inhibitors for severely hypertensive dogs (SBP > 200 mm Hg). Dosages typically range from 0.1-0.5 mg/kg orally every 24 hours. CCBs cause vasodilation, lowering blood pressure. However, CCB monotherapy in dogs should generally be avoided as it can preferentially dilate the renal afferent arteriole, potentially increasing pressure in the glomerulus. When combined with a RAAS inhibitor, this effect is often mitigated.
Other Medications
- Alpha-blockers (e.g., Prazosin, Phenoxybenzamine): These may be used for specific conditions like hypertension associated with pheochromocytoma. Prazosin (0.5-2 mg/kg orally every 8-12 hours) is a common choice.
- Beta-blockers (e.g., Propranolol, Atenolol): While they can control heart rate in some conditions, beta-blockers typically have negligible direct antihypertensive effects in dogs and are not used as sole agents for hypertension management.
- Direct Vasodilators (e.g., Hydralazine): These drugs rapidly dilate blood vessels and may be used in emergency situations or when other medications are insufficient. Hydralazine (0.5-2 mg/kg orally every 12 hours) can be effective.
- Aldosterone Antagonists (e.g., Spironolactone): These are particularly useful for hypertension stemming from primary hyperaldosteronism.
- Diuretics: While common in human hypertension treatment, diuretics are not first-choice drugs for dogs, especially those with CKD, due to the risk of dehydration. They might be considered in cases of volume expansion (e.g., edema).
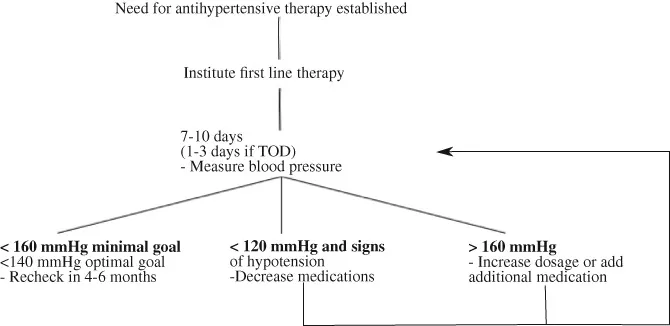 A management chart illustrating a stepwise approach to canine hypertension, including repeat blood pressure measurements and medication adjustments.
A management chart illustrating a stepwise approach to canine hypertension, including repeat blood pressure measurements and medication adjustments.
Important Considerations for Medication
When your dog is prescribed medication for high blood pressure, several factors are vital for successful treatment. Firstly, consistency in administering the medication at the prescribed dosage and frequency is paramount. Missing doses or inconsistent timing can hinder blood pressure control. Secondly, understanding potential side effects is important; while many dogs tolerate these medications well, some may experience lethargy, gastrointestinal upset, or excessive lowering of blood pressure (hypotension). Signs of hypotension include weakness, dizziness, or collapse. Regular follow-up visits with your veterinarian are critical for monitoring your dog’s blood pressure, assessing the effectiveness of the medication, and checking for any adverse reactions or changes in kidney function, especially when treating severe conditions like those addressed by albuterol for dogs with collapsed trachea. These visits also allow your vet to adjust the medication regimen as needed to ensure optimal control and minimize risks. The effectiveness of any medication, including pain medication for hip dysplasia in dogs, can vary from dog to dog, necessitating a personalized approach to veterinary care.
Managing Hypertensive Emergencies in Dogs
In rare cases, a dog may experience a “hypertensive emergency,” where a sudden, marked increase in blood pressure is accompanied by acute, ongoing target organ damage. This is a critical situation requiring immediate and aggressive treatment, often in a 24-hour care facility. Signs of a hypertensive emergency typically involve severe ocular issues (e.g., acute blindness, retinal detachment) or neurological signs (e.g., seizures, coma, severe disorientation).
The goal in such emergencies is an incremental decrease in blood pressure—approximately 10% in the first hour and another 15% over the next few hours—rather than rapid normalization. This prevents hypoperfusion to organs that have adapted to chronically high pressures. Parenteral (injectable) medications that can be quickly titrated to effect are preferred, such as fenoldopam, labetalol, hydralazine, or nitroprusside. Continuous monitoring of blood pressure is essential to ensure a safe reduction and avoid dangerous hypotension. Once blood pressure is stable for 12-24 hours, oral medications can be slowly introduced as parenteral drugs are tapered. For patients without acute TOD but with SBP ≥ 180 mm Hg, oral medications like hydralazine or amlodipine can be used for rapid, but controlled, blood pressure reduction.
Conclusion
Managing high blood pressure in dogs is an evolving field, and while significant advancements have been made, continuous research helps refine our understanding and treatment approaches. As a pet owner, your active participation and adherence to veterinary recommendations are vital. By understanding the causes, diagnosis, and treatment options for canine hypertension, you can play a crucial role in preventing target organ damage and ensuring your dog lives a healthier, longer life. Always consult with your veterinarian for a personalized diagnosis and treatment plan for your beloved companion.
References:
- Acierno MJ, Brown S, Coleman AE, et al. ACVIM consensus statement: Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. J Vet Intern Med. 2018;32:1803–1822.
