Zoonotic hookworms are parasitic organisms that typically reside in animals such as dogs and cats. However, these parasites have the ability to transmit to humans, entering the body through the skin and causing a condition known as cutaneous larva migrans (CLM). This occurs when the immature hookworms, or larvae, burrow into unprotected human skin. This typically happens when individuals walk barefoot or have exposed skin in contact with soil or sand contaminated with animal feces. Understanding the life cycle and transmission methods of these parasites is crucial for pet owners and travelers alike.
How Zoonotic Hookworms Spread
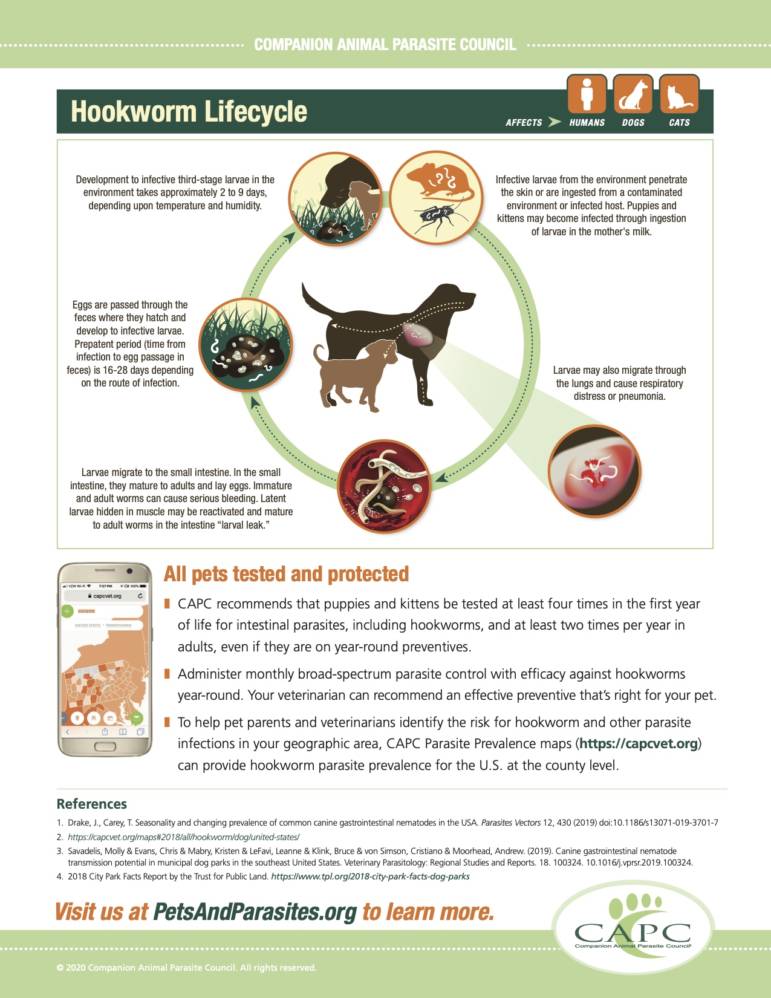
The transmission of zoonotic hookworms follows a distinct cycle that involves both animals and the environment. Infected animals, commonly dogs and cats, excrete hookworm eggs in their feces. These eggs then mature and hatch in the soil or sand, releasing infective larvae. When humans come into contact with contaminated soil or sand, particularly with bare skin, these larvae can attach to the skin and begin burrowing. This process highlights the importance of prompt disposal of animal waste to prevent eggs from contaminating the environment and hatching.
Signs and Symptoms of Cutaneous Larva Migrans (CLM)
Once zoonotic hookworm larvae penetrate human skin, they cause CLM. The most common and prominent symptoms include severe itching and the appearance of raised red lines on the skin, often referred to as tracks. These tracks are a direct result of the larvae burrowing through the skin. Fortunately, these symptoms typically resolve on their own within several weeks as the parasite eventually dies. In rarer instances, certain types of hookworms may migrate to deeper tissues, potentially affecting the intestines, lungs, or even the eyes, though this is uncommon with zoonotic hookworms.
Risk Factors Associated with Zoonotic Hookworm Infection
Individuals who have traveled to tropical regions are at a higher risk of contracting CLM, as the larvae of dog and cat hookworms can thrive in the soil of these climates. Walking barefoot in soil or sand in these areas significantly increases the likelihood of infection. While more prevalent in tropical zones, zoonotic hookworms can be found globally. For example, in the United States, they are more frequently diagnosed on the East Coast compared to the West Coast. This geographical distribution underscores the need for caution in various environments.
Prevention Strategies for Zoonotic Hookworms
Preventing zoonotic hookworm infection involves a combination of responsible pet ownership and personal protective measures. Promptly disposing of animal waste is a primary preventive step, as it minimizes the opportunity for eggs to contaminate soil and hatch. Ensuring that dogs and cats receive regular veterinary care, including deworming treatments when necessary, is also vital in controlling the spread of these parasites. For humans, wearing shoes when walking in areas where contamination is suspected and avoiding direct skin contact with contaminated sand or soil are essential. When traveling to tropical or subtropical climates, especially those with beaches, it is strongly advised to wear protective footwear and use mats or other barriers to prevent direct skin contact with the sand or soil. If you suspect your pet may have parasites, seeking veterinary advice promptly is recommended.
Diagnosis and Treatment of CLM
If you experience symptoms suggestive of CLM, consulting a healthcare provider is important. Diagnosis typically involves a visual examination of the skin, where a healthcare provider will look for the characteristic itchy, red tracks, most commonly found on the legs or feet. Currently, there is no specific blood test for zoonotic hookworm infection. However, your provider may inquire about your recent travel history, which can aid in reaching an accurate diagnosis.
In most cases, zoonotic hookworm infections resolve naturally within approximately 5 to 6 weeks as the causative parasites die off, often without the need for medical intervention. Nevertheless, in some instances, a healthcare provider may prescribe antiparasitic drugs to help eliminate the hookworms more quickly or antibiotics to treat any secondary bacterial infections that may have developed in the damaged skin. Following your healthcare provider’s recommendations is crucial for effective management and recovery.